This bionic hand is fused to a woman’s bones, muscles, and nerves
This article is an installment of Future Explored, a weekly guide to world-changing technology. You can get stories like this one straight to your inbox every Thursday morning by subscribing here.
More than 20 years ago, a Swedish woman named Karin was in a farming accident that led to the loss of her right hand a few inches above the wrist. Afterward, she endured severe pain coming from her phantom limb (the place where her hand used to be).
“It felt like I constantly had my hand in a meat grinder, which created a high level of stress and I had to take high doses of various painkillers,” said Karin.
On top of dealing with this pain, she was also stuck navigating life with just one hand most of the time — the only prosthetics available to her were uncomfortable and hard to control, meaning they did little to help her with daily life.
“[It’s] a promising testament to the potential life-changing capabilities of this novel technology.”
Max Ortiz Catalan
In 2018, researchers at the Center for Bionics and Pain Research (CBPR) in Sweden used a unique combination of surgery and AI to connect Karin’s skeleton, muscles, and nerves to a bionic hand, and it changed her life, reducing her pain and giving her more control over her prosthetic.
“Karin was the first person with below-elbow amputation who received this new concept of a highly integrated bionic hand that can be used independently and reliably in daily life,” said Max Ortiz Catalan, founder of the CBPR and lead author of a paper on Karin’s case.
“The fact that she has been able to use her prosthesis comfortably and effectively in daily activities for years is a promising testament to the potential life-changing capabilities of this novel technology for individuals facing limb loss,” he continued.
The bionic hand
The key to Karin’s success lies in how the researchers connected the bionic hand to her residual limb (the part of the arm left after the amputation) on multiple levels.
First, she underwent a procedure, known as “osseointegration,” during which titanium rods were implanted in the radius and ulna bones of her arm. These rods now protrude from the end of the residual limb, and Karin uses them to attach and detach her bionic hand.
Osseointegration eliminates the need for a socket, the cup-like device that typically connects a prosthetic to the residual limb. Sockets can cause sweating, skin irritation, and other issues, and because they press on nerves, they can also increase the pain.

Surgeons also removed jumbles of nerve cells called “neuromas” from the ends of the three main nerves in Karin’s residual limb. These structures often form after an amputation and have been linked to stump pain and phantom limb pain.
Using electrodes and muscle grafts taken from Karin’s leg, the researchers connected the nerves and muscles in her residual limb to the titanium rods. This allows for bi-directional communication between the bionic hand and Karin’s residual limb: the muscles and nerves in her arm can send signals to it, and it can send signals back to them.
With conventional socket-attached bionic hands, electrodes stuck to the surface of the residual limb detect and translate muscle movements into commands for the prosthetic. Those electrodes can be affected by sweat, friction from clothes, and other external factors, leading to inconsistent readings and unreliable control of the bionic device.

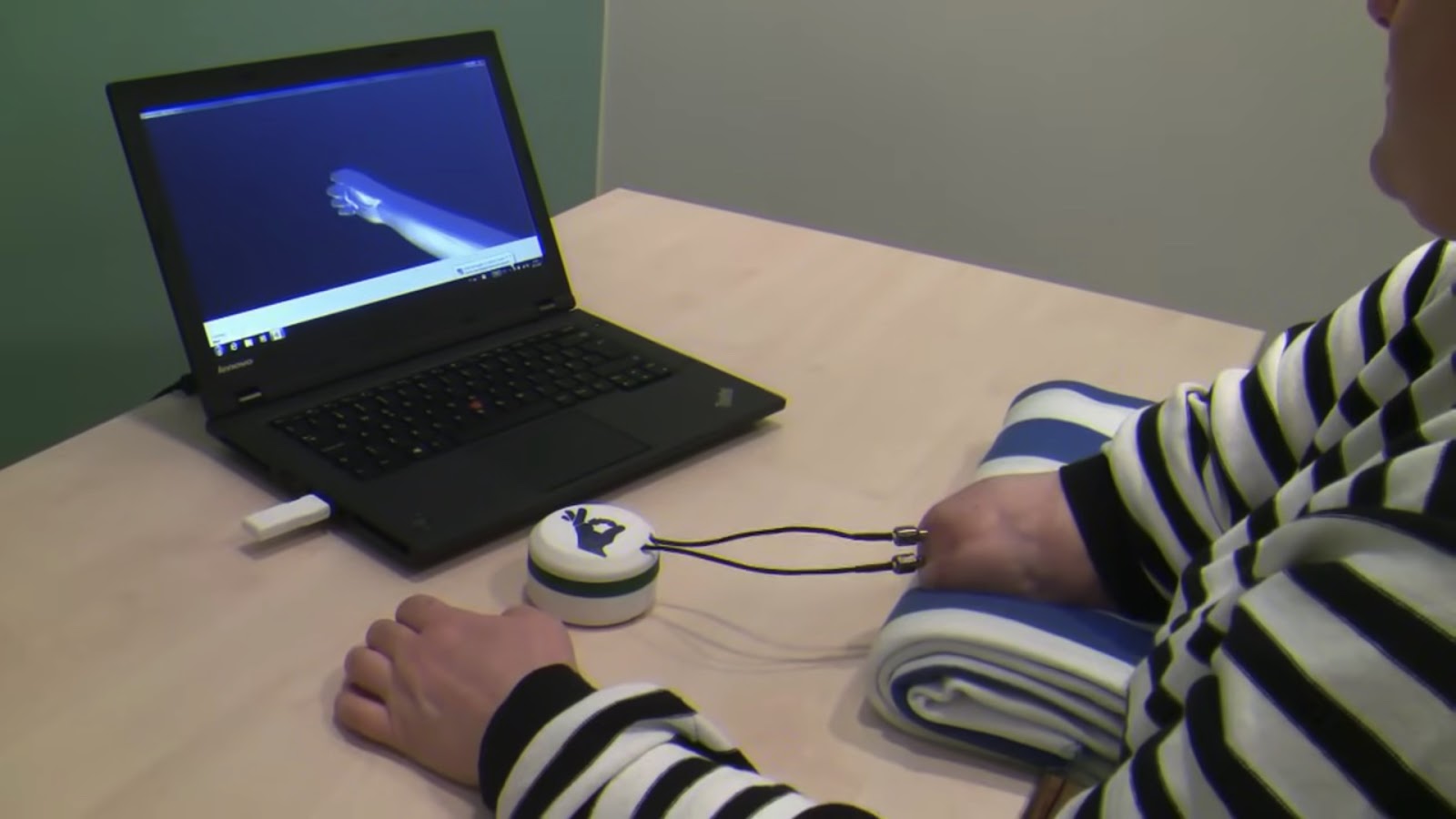
After the surgery, Karin used computer simulations to train AI algorithms to translate the signals in her arm when she tried to move her amputated hand into commands for the bionic hand.
She also learned how to interpret electric pulses that are sent from sensors in the forefinger and thumb of her bionic hand back to her arm. Based on these signals, she can determine how much force is required to effectively grip an object between the digits.
The impact
On two tests used to gauge the functionality of a prosthetic (the ACMC and the SNAP), Karin scored higher with the new integrated system than the socket and surface electrode system she was using before, even though it was attached to the same actual bionic hand she was using previously: Ottobock’s MyoHand Variplus Speed.
When she wasn’t completing tests, Karin was given the option of using a more advanced bionic hand — Prensilia’s Mia Hand — which has multiple degrees of freedom, unlike the MyoHand.
Based on her experience with both bionic hands over about two years, she completed questionnaires assessing her quality of life, perception of her disability, and pain levels before and after the intervention, and all improved. On a scale of 0 to 10, the average intensity of her phantom limb pain went from a 5 to a 3, while the pain in her residual limb dropped from a 6 to a 0.
“For me, this research has meant a lot, as it has given me a better life… [I have] better control over my prosthesis, but above all, my pain has decreased,” said Karin. “Today, I need much less medication.”
The big picture
Even though Karin’s highly integrated bionic hand is a huge upgrade, it still isn’t nearly as functional as the hand she lost in the farming accident.
That’s because the human hand is one of the most complex structures in nature — roboticists still haven’t managed to perfectly replicate it, and they don’t have to worry about integrating their mechanical hands with a human brain and nervous system, like bionics developers do.
“We can restore human function in an unprecedented way.”
Rickard Brånemark
Still, Karin’s experience shows that changing how we integrate existing bionics with the human body can have a huge impact on their functionality and greatly improve the lives of the people using them.
Making such approaches accessible to anyone who wants them will be the next hurdle — a bionic hand can cost tens of thousands of dollars, and the surgeries and training Karin received during the study would likely add significantly to the overall cost in the US.
“By combining osseointegration with reconstructive surgery, implanted electrodes, and AI, we can restore human function in an unprecedented way,” said lead surgeon Rickard Brånemark.
“The below-elbow amputation level has particular challenges, and the level of functionality achieved marks an important milestone for the field of advanced extremity reconstructions as a whole,” he continued.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].






