Exercise boosts the brain — and mental health
Mental health disorders such as depression and anxiety aren’t easy to treat. Medications help many but have a high failure rate and may bring nasty side effects. Talk therapy is time-consuming and expensive. And neither approach is suited to preventing the disorders from developing in the first place. But many people overlook another option that, when it works, can be one of the most effective, least disruptive and cheapest ways of managing mental health disorders: exercise.
It’s hardly news that exercise is good for your physical health, and has long been extolled for mental health as well. But researchers are now making progress in understanding how, exactly, exercise may work its mental magic.
Exercise, they are learning, has profound effects on brain structure itself, and especially in regions most affected by depression and schizophrenia. It also provides other, more subtle benefits such as focus, a sense of accomplishment and sometimes social stimulation, all of which are therapeutic in their own right. And while more is generally better, even modest levels of physical activity, such as a daily walk, can pay big dividends for mental health.
“It’s a very potent intervention to be physically active,” says Anders Hovland, a clinical psychologist at the University of Bergen in Norway.
But that knowledge has barely begun to percolate into practice, says Joseph Firth, a mental health researcher at the University of Manchester in the UK. Just ask a hundred people receiving mental health care how many are getting exercise prescriptions as part of that care. “You wouldn’t find many,” Firth says.
Exercise — a tool against depression
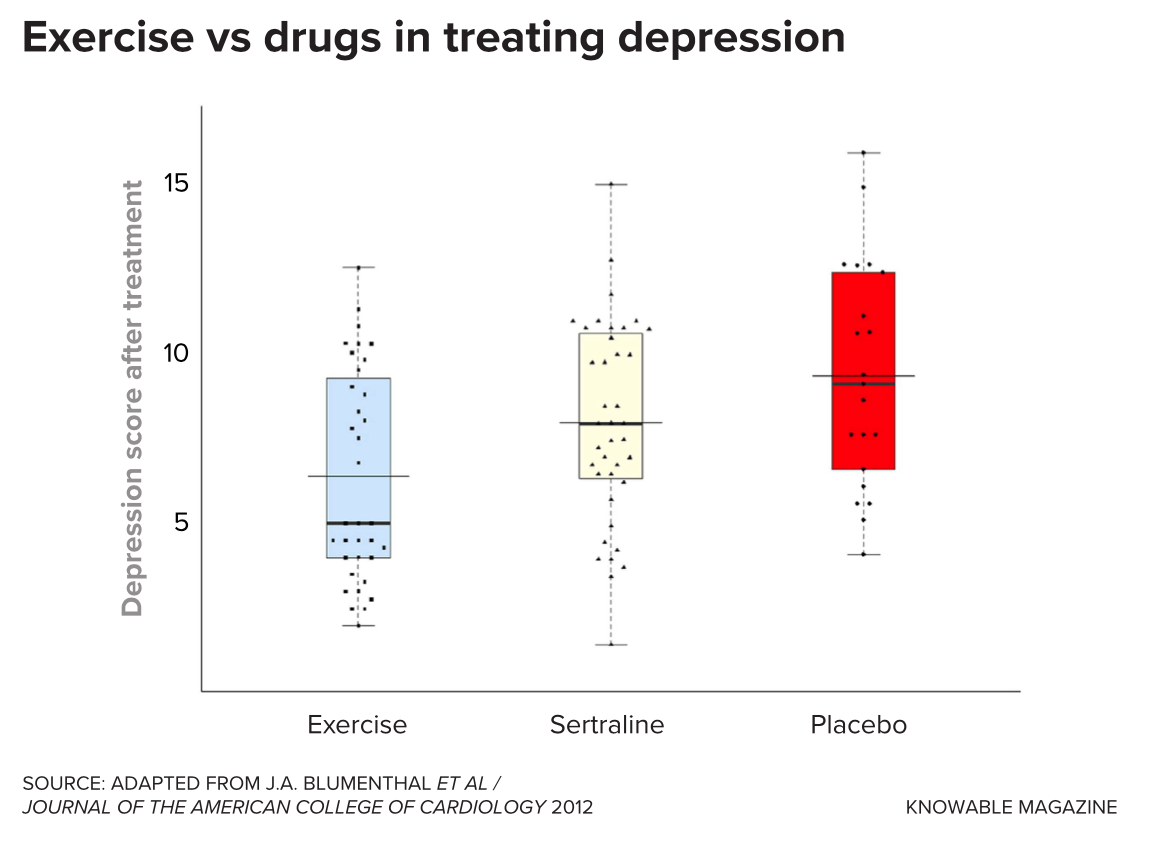
Some of the strongest evidence for the mental benefits of exercise centers on depression. In 2016, Hovland and his colleagues searched the published literature and identified 23 clinical trials that tested the effectiveness of exercise in treating depression. Exercise was clearly effective and, in few studies, on par with antidepressant drugs, the researchers concluded.
And exercise offers several advantages. For one thing, antidepressant medications generally take several weeks or months to show their full effect. Exercise can improve mood almost immediately, making it a valuable supplement to frontline treatments such as drugs or therapy, notes Brett Gordon, an exercise psychology researcher at the Penn State College of Medicine. Plus, he says, exercise can counteract some of the unpleasant side effects of antidepressants, such as weight gain.
In addition, exercise has few of the negative side effects that are so common in drug therapies for depression and other disorders. “Many people who have mental health concerns are not enthusiastic about starting a medication for the rest of their lives, and are interested in pursuing other options. Exercise might be one of those options,” says Jacob Meyer, an exercise psychologist at Iowa State University.
There’s now emerging evidence that exercise also seems to help in treating or avoiding anxiety disorders, including post-traumatic stress disorder (PTSD), and possibly other serious psychotic conditions as well. “The more we do these studies, the more we see that exercise can be valuable,” says Firth.
There’s a flip side to this coin that’s especially relevant during the Covid-19 pandemic: If exercise stabilizes mental health, then anything that prevents people from working out is likely to destabilize it. To test this, Meyer and his colleagues surveyed more than 3,000 Americans about their activity before and during the pandemic. Those who became less active because of Covid reported more depression and poorer mental health, they found. (Ironically, those who had not exercised regularly pre-Covid didn’t report much change. “When you’re already at zero, where do you go?” says Meyer.)
But researchers are still figuring out exactly how muscular exertion acts on the brain to improve mental health. For most biomedical questions like this, the first stop is animal experiments, but they aren’t as useful in studies of mental health issues. “Psychological health is so uniquely human that it can be hard to make a good jump from animal models,” says Meyer.
Exercise and a healthy brain
Scientists have come up with a few ideas about how exercise enhances mental health, says Patrick J. Smith, a psychologist and biostatistician at Duke University Medical Center in North Carolina, who wrote about the subject in the 2021 Annual Review of Medicine with his Duke colleague Rhonda M. Merwin. It doesn’t seem to have much to do with cardiovascular fitness or muscular strength — the most obvious benefits of exercise — since how hard a person can work out is only weakly associated with their psychological health. Something else must be going on that’s more important than mere fitness, says Smith.
One likely possibility is that exercise buffs up the brain as well as the body. Physical exercise triggers the release of a protein known as brain-derived neurotrophic factor (BDNF). BDNF is one of the key molecules that encourage the growth of new brain cells — including, possibly, in the hippocampus, a brain region important in memory and learning. Since the hippocampus tends to be smaller or distorted in people with depression, anxiety and schizophrenia, boosting BDNF through exercise may be one way physical activity might help manage these conditions.
Sure enough, studies show that people with depression have lower levels of BDNF — and, notably, one effect of antidepressant drugs is to increase production of that molecule. Researchers have not yet shown directly that the exercise-associated increase in BDNF is what reduces depressive symptoms, but it remains one of the most promising possibilities, says Hovland.
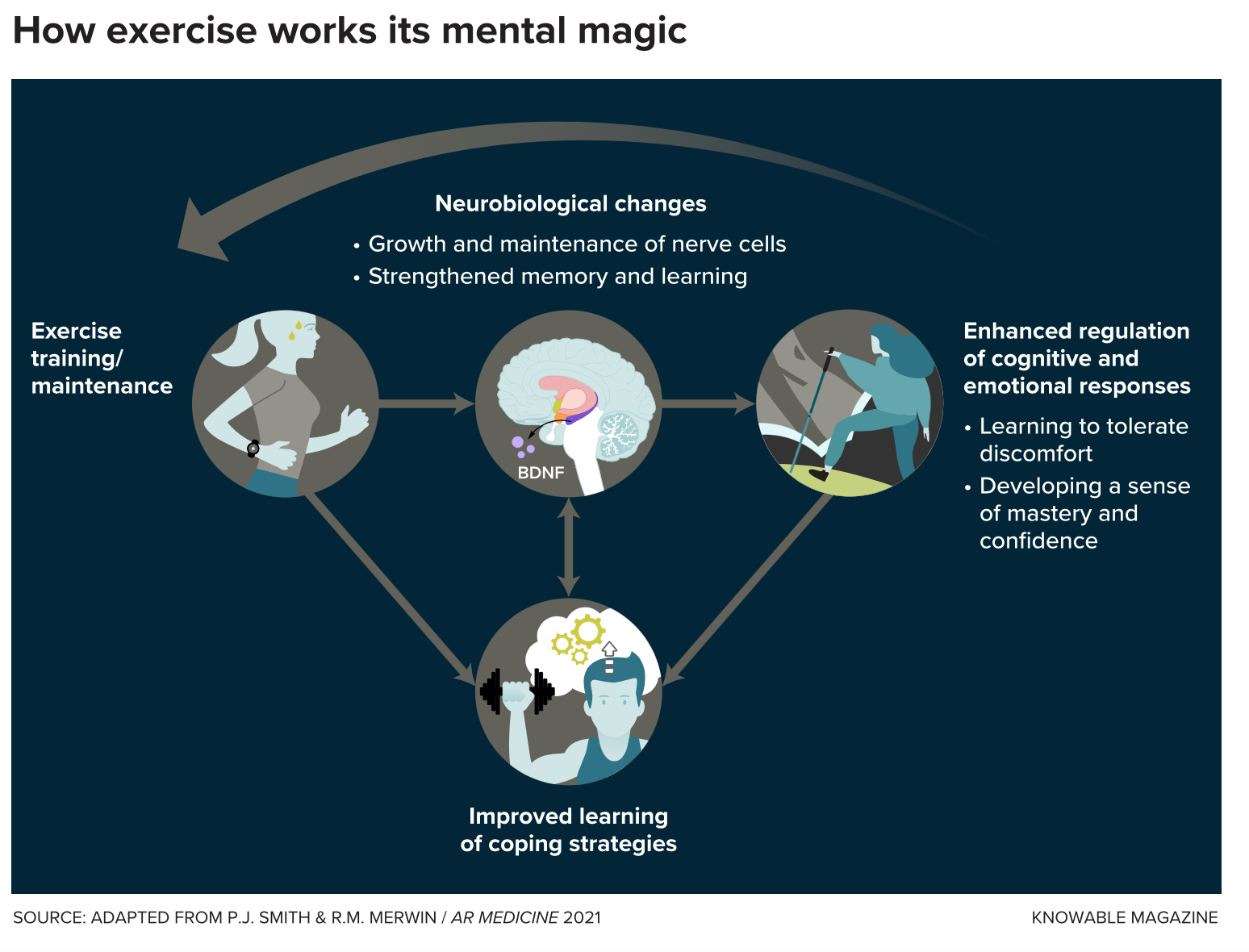
Exercise may also help anxiety disorders. The brain changes prompted by BDNF appears to enhance learning, which is an important part of some anti-anxiety therapies. This suggests that exercise may be a useful way of improving the effectiveness of such therapies. One of the standard therapies for PTSD, for example, involves exposing patients to the fear-causing stimulus in a safe environment, so that the patients learn to recalibrate their reactions to trauma-linked cues — and the better they learn, the more durable this response might be.
Kevin Crombie, an exercise neuroscientist now at the University of Texas at Austin, and his colleagues tested this idea in the lab with 35 women with PTSD. Researchers first taught the volunteers to associate a particular geometric shape with a mild electric shock. The next day, the volunteers repeatedly saw the same shape without the shock, so that they would learn that the stimulus was now safe. A few minutes later, half the volunteers did 30 minutes of moderate exercise — jogging or uphill walking on a treadmill — while the other half did only light movement, not enough to breathe heavily.
The following day, those who had exercised were less likely to anticipate a shock when they saw the “trigger” shape, Crombie found — a sign that they had learned to no longer associate the trigger with danger. Moreover, those volunteers who showed the greatest exercise-induced increases in BDNF also did best at this relearning.
Although the evidence is not yet definitive, a few studies have suggested that regular exercise may lead to better outcomes in patients with schizophrenia too. Vijay Mittal, a psychologist at Northwestern University, wondered whether working out also might prevent people from developing the disorder in the first place.
Mittal works with teenagers who are at high risk of psychotic disorders such as schizophrenia, but who have not yet progressed to the full-on disorder. In the past two decades, researchers have gotten much better at recognizing such individuals just as they begin to display the earliest signs of illness, such as seeing shadows out of the corner of their eye or hearing indistinct voices when no one is home.
For about 10 percent to 33 percent of these teens, these early signs turn into something more serious. “A shadow might turn into a person,” says Mittal. “A whisper might turn into words. A suspicion that someone is following them might turn into the belief that the government is after them.”
Previously, Mittal had found that the hippocampus is different in at-risk teens who later slid down this slippery slope than in those who didn’t. He wondered whether exercise might help bolster the hippocampus and avert the slide. So his team tested this notion in a sample of 30 high-risk teens, half of whom followed a regimen of aerobic exercise twice a week for three months. (The other half, the control group, were told they were on the wait list for the exercise program.) The researchers used brain scans to look at participants’ hippocampus before and after the program.
The experiment has just concluded, and Mittal is still analyzing the results, which he calls promising. He cautions, however, that exercise is not a panacea. Schizophrenia is a diverse disease, and even if physical activity proves to be protective for some at-risk people, not all are likely to respond to it in the same way. “It’s really important to remember that these disorders are complicated. I’ve worked with people who exercise a lot and still have schizophrenia,” he says.
If Mittal’s work pans out, exercise may allow mental health workers to help a group that isn’t easily treated with drugs. “Someone who’s just at risk of a psychotic disorder, you can’t just give them medication, because that has risks too,” says Firth. “It would be fantastic to have something else in our arsenal.”
Exercise almost certainly has other effects on the brain, too, experts agree. For example, exercise stimulates the release of endocannabinoids, molecules that are important in modifying the connections between brain cells, the mechanism that underlies learning. This may provide another way of enhancing the learning that underlies successful treatment for depression, PTSD and other mental disorders. Indeed, Crombie’s study of exercise in a simplified model of PTSD therapy measured endocannabinoids as well as BDNF, and increases in both were associated with stronger learning responses.
And physical activity also moderates the body’s response to stress and reduces inflammation, both of which could plausibly help improve brain health in people with mental illness. “We have just scratched the surface,” says Hovland.
Moving the body, engaging the mind
But changing the structure of the brain isn’t the only way physical activity can be beneficial for those suffering from mental health conditions. The habit of exercise can itself be beneficial, by altering people’s thought patterns, says Smith.
For people with mental health issues, simply doing something — anything — can be helpful in its own right because it occupies their attention and keeps them from ruminating on their condition. Indeed, one survey of the published literature found that placebo exercise — that is, gentle stretching, too mild to cause any physiological effect — had almost half the beneficial effect on mental health as strenuous exercise did.
Besides just occupying the mind, regular workouts also give exercisers a clear sense of progress as their strength and fitness improves. This sense of accomplishment — which may be especially notable for weight training, where people make quick, easily measurable gains — can help offset some of the burden of anxiety and depression, says Gordon.
If so, playing a musical instrument, studying a language and many other activities could also help people cope with mental health conditions in a similar way. But exercise does more than that, making it one of the best choices for managing mental health. “You can see benefits from doing anything, but the exercise may confer greater benefits,” says Firth.
For one thing, relatively strenuous exercise teaches people to put up with short-term discomfort for long-term gain. People who suffer from anxiety disorders such as PTSD or panic attacks often show a reduced ability to tolerate mental discomfort, so that experiences most people would cope with result in uncontrolled anxiety instead. There’s now emerging evidence that regular exercise builds tolerance for internal discomfort, and this may explain part of its benefit in managing these conditions, Smith says.
Using exercise as a mental health treatment brings some challenges, however. “People with mental illness are also at higher risk of struggling with low motivation,” Firth says. This can make it difficult to organize and stick with an exercise program, and many patients need additional support.
This is often difficult, because psychologists, psychiatrists and other mental health workers are often already overburdened. Plus, prescribing and supervising exercise hasn’t traditionally been within these practitioners’ purview. “We’re telling people, ‘Hey, exercise is helpful,’ but we’re telling it to people who can’t really incorporate it because they often don’t get any training,” Firth says. Exercise referral schemes, which link patients with fitness specialists and structured programs at community leisure centers, have been used in the UK and other places to encourage exercise in people with physical conditions such as obesity and diabetes. A similar approach could be valuable for mental health conditions, Firth says.
Therapists can also help patients persist for the long term by tailoring their exercise prescriptions to each individual’s capabilities. “I always tell patients that doing anything is better than doing nothing, and the best exercise for you is the one you’ll actually do,” Smith says.
The secret, he suggests, is to make sure people stop exercising before they’ve done so much it makes them feel exhausted afterward. “When you feel like crap after exercise, you’re not going to want to do it,” he says, because the brain tags the activity as something unpleasant. It’s far better to have the patient quit while they still have a positive feeling from the workout. “Without even realizing it, their brain tends to tag that activity as something more pleasurable. They don’t dread it.”
Even light activity — basically just moving around now and then during the day instead of sitting for hours at a time — may help. In one study of more than 4,000 adolescents in the UK, Aaron Kandola, a psychiatric epidemiologist at University College London, and his colleagues found that youths who undertook more light activity during the day had a lower risk of depressive symptoms than those who spent more time sitting.
“What we really need are big exercise trials where we compare different amounts against each other,” says Kandola. “Instead, what we have are different studies that used different amounts of activity.” That makes precise recommendations difficult, because each study varies in terms of its patient populations and methods, and follows results for a different length of time. As researchers learn more about the mechanisms linking exercise to mental health, they should be able to refine their exercise prescriptions so that patients are best able to manage their illnesses.
And exercise has powerful benefits for people with mental illness that go beyond its effects on the illnesses themselves. Many struggle with related issues such as social withdrawal and a reduced capacity for pleasure, says Firth. Standard medications reduce some symptoms but do nothing to address these other problems. Exercise — especially as part of a group — can help boost their mood and enrich their lives.
Even more important, people with serious mental illnesses such as severe depression and schizophrenia also are more likely to have significant physical health issues such as obesity, heart disease and other chronic diseases, and as a result their life expectancy is 10 to 25 years lower than that of unaffected people.
“Reducing those health risks is really paramount at the moment,” says Kandola. “That’s the big appeal of exercise: We already know it can improve physical health. If it does have mental health benefits as well, it can be quite an important addition to treatment.”
This article originally appeared in Knowable Magazine, a nonprofit publication dedicated to making scientific knowledge accessible to all. Sign up for Knowable Magazine’s newsletter.