New cancer treatment uses “hot blood cells” to target tumors
One of the biggest challenges to treating cancer is getting drugs to tumors.
Many drugs that look promising in a Petri dish end up failing simply because they can’t get the tumor — or can’t get there without causing a lot of collateral damage.
Now, Chinese researchers have developed a new cancer treatment that may be better at homing in on tumors — thanks to modified blood cells that heat up when exposed to light.
A Combination Therapy
The new cancer treatment combines existing two therapies — immunotherapy and photothermal therapy — into one.
The mice that received the new cancer treatment were all still alive at the end of the study.
Immunotherapy uses a patient’s own immune system as a weapon against cancer — this might involve a vaccine or immunostimulant drugs.
Photothermal therapy is more experimental.
Nanoparticles, designed to heat up when exposed to certain wavelengths of light, are injected into a patient’s body. By focusing light on a tumor, doctors can get the nanoparticles to heat up in that exact location and kill the cancer cells.
The New Cancer Treatment
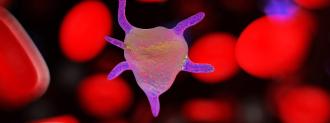
For their new cancer treatment, the researchers modified blood platelets to contain both an immunostimulant drug (which calls the body’s immune cells to attack) and photothermal nanoparticles.
They tried the modified blood cells against nine different mouse models of cancer. When they shone near-infrared light on the animals’ tumors, the platelets near the tumors heated up.
That caused the cells to release the immunostimulant drug, which then triggered an immune response — right on target.
Some of the platelets were also broken into smaller “proplatelets” by the heat. Those blood cell fragments were tiny enough to get deep inside the tumor, bringing the immunostimulant drug with them.
The heat also damaged blood vessels near the tumor — and when blood vessels are damaged, platelets swoop in to repair them by clotting. That meant the therapy itself brought more of the cancer-fighting platelets to the tumor site, where they could be activated by light.
Making the Leap From Mice
The new cancer treatment stopped tumor development almost completely in the mice, and at the end of the 100-day experiment, they were all still alive.
By comparison, the mice that didn’t get both therapies didn’t live past the 50-day mark.
“These results show great promise for utilization of this novel biomimetic platelet platform in high-performance and combined anticancer therapies,” researcher Ma Guanghui said in a press release.
If the results translate from mice to humans (always a big if), cancer patients might one day have their own hot blood used as a weapon against their disease.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].